Cervical Stenosis
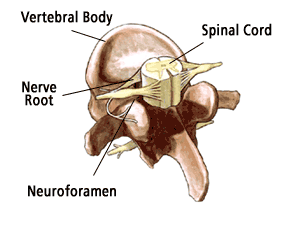
A common cause of neck pain, especially in older patients, is cervical stenosis. Cervical stenosis is a narrowing of the spinal canal in the neck area or upper part of the spine. This narrowing places pressure on the spinal cord. While some patients are born with this narrowing, most cases of cervical stenosis occur to patients over the age of 50 and are the result of aging and "wear and tear" on the spine.
Many patients with cervical stenosis have a history of some kind of injury or trauma to the neck, however this trauma may have occurred many months or even years before the onset of stenosis symptoms.
Symptoms
The symptoms of cervical spinal stenosis may include the following:
- Neck pain; not always severe.
- Pain, weakness, or numbness in the shoulders, arms, and legs.
- Hand clumsiness.
- Gait and balance disturbances.
- Burning sensations, tingling, and pins and needles in the involved extremity, such as the arm or leg.
- In severe cases, bladder and bowel problems.
- Although rare, severe cases can also cause significant loss of function or even paraplegia.
Diagnosis
Good treatment is always based on an accurate diagnosis. The comprehensive diagnostic process includes:
- Medical history. Your doctor will talk to you about your symptoms, how severe they are, and what treatments you have already tried.
- Physical examination. You will be carefully examined for limitations of movement, problems with balance, and pain. During this exam, the doctor will also look for loss of reflexes in the extremities, muscle weakness, loss of sensation or other signs of spinal cord damage.
- Diagnostic tests. Generally, doctors start with plain x-rays, which enable them to rule out other problems such as tumors and infections. CT scans and MRIs give three-dimensional views of the cervical spine and can help detect osteophytes (bony growths) and herniated discs. Occasionally doctors use a myelogram. This is a test that involves injecting liquid contrast dye into the spinal column to show where the spinal cord pressure is occurring.
Non - Operative Treatment
Most cases of cervical stenosis are successfully treated with non-surgical techniques such as pain and anti-inflammatory medications. Depending on the extent of nerve involvement, some patients may need to temporarily restrict their activities and wear a cervical collar or neck brace for a time. However, most patients only need to rest for a brief time. Physical therapy exercises will also be prescribed to help strengthen and stabilize the neck as well as build endurance and increase flexibility.
Surgical Treatment
If non-surgical measures do not work, your doctor may recommend surgery to treat your stenosis. There are a number of surgical techniques that can be used to treat this condition. The goal of each of these surgical decompression treatments is to widen the spinal canal and relieve the pressure on the spinal cord by removing or trimming whatever is causing the compression. However, since all surgical procedures carry a certain amount of risk, your doctor will discuss all of your options with you before deciding which procedure is best for you.
The most common surgery for cervical stenosis is called a decompressive laminectomy in which the laminae (roof) of the vertebrae are removed, creating more space in the spinal canal for the nerves. If only a portion of the laminae need to be removed, it is called a laminotomy.
Your surgeon may also consider performing a posterior laminoplasty. This technique helps to retain spinal stability while also expanding the spinal canal.
If there are any herniated or bulging discs, these may also be removed (this is called a discectomy) to increase canal space. Sometimes the foramen (the area where the nerve roots exit the spinal canal) also need to be enlarged. This procedure is called a foraminotomy.
For those patients who need surgical repair on more than one level or who have significant spinal instability, spinal fusion may be done in addition to the decompression surgery. This involves taking a small piece of bone (usually from the hip) and grafting it onto the spine. Spinal hardware (called instrumentation) such as plates and screws are used to support the spine and provide additional stability. In most cases, we can determine ahead of time if fusion surgery is necessary. If it is, we will discuss this with you so that you are aware of what is being done.
Recovery
Most patients can begin getting out of bed on the same day surgery is performed! Activity is gradually increased and patients are typically able to go home within a few days after their procedure, depending on the extent of the surgery. As with most surgeries, there will be some pain after the procedure. However, doctors have pain medications available that will help keep you comfortable. Doctors today take pain management very seriously!
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a week or two after surgery. Other techniques for reducing pain and increasing flexibility will be discussed with you before you leave for home. When you can return to work and other activities such as sports and driving will also be discussed with you by your doctor.